
In the case of thoracic osteochondrosis, the organs associated with the areas of the spinal cord, located at the level of the affected chest region and below, often suffer. Violation of the normal activity of the spine leads to immobility of the arms, legs and torso as a whole, dysfunction of the pelvic organs, respiratory muscles and internal organs.
Osteochondrosis is a degenerative-dystrophic disease of the spine, which is based on a change in the intervertebral discs with involvement in the pathological process of neighboring vertebrae and intervertebral joints with the entire ligamentous apparatus.
Features of the anatomy of the spine
Mobility and stability, elasticity and elasticity of the spine largely depend on the intervertebral discs, which are one of the types of cartilaginous connection between the bones and provide a strong connection between the bodies of neighboring vertebrae. The total length of the intervertebral discs is one quarter of the length of the spine.
The most important function of the discs is to reduce the vertical load on the vertebrae. The disc is made up of three parts:
- hyaline plates (closely adjacent to the vertebrae);
- nucleus pulposus (fills the space between the plates);
- fibrous ring (surrounds the nucleus from the outside).
The nucleus contains cartilage cells, tightly interwoven collagen fibers and chondrin (proteoglycans). The anterior surface of the discs is covered by the anterior longitudinal ligament, which is tightly fused with the vertebrae and freely turns over the discs. The posterior longitudinal ligament is firmly fused with the surface of the disc and forms the anterior wall of the spinal canal. The intervertebral disc does not have its own blood supply, so it feeds on substances that come by diffusion from the vertebral bodies.
The distribution of vertical loads in the spine occurs due to the elastic properties of the discs. Under the effect of pressure, the nucleus pulposus expands and the pressure is redistributed to the annulus fibrosus and the hyaline plates. During movement, the core moves in the opposite direction: when flexed - to convexity, when flexed - forward. When the spine moves, the muscles, ligaments and discs are involved in the work. Therefore, a violation of one link leads to a violation of the entire kinetic chain.
Causes and mechanism of disease development
In the development of osteochondrosis, the mechanical effect on the spine plays a special role. Under the influence of unfavorable static and dynamic loads, the nucleus pulposus gradually loses its elastic properties (as a result of the depolymerization of polysaccharides), forms protrusions and sequesters.
The process of disc degeneration is influenced by a genetic predisposition, which provokes the development of changes in the neuromuscular apparatus of the back, a change in the structure of glycosamines and a violation of the distribution of collagen fibers in the disc. The genetic factor is paramount in the occurrence of thoracic osteochondrosis, subject to increased functional activity.
Risk factors for the development of degenerative changes in the spine include the anatomical features of the discs, which are evolutionary imperfections. One of these characteristics is the nutritional characteristics of the structures. In the human body, the disc is made up of poorly perfused tissue. The closing of blood vessels occurs already in childhood. After nutrition occurs due to the diffusion of substances through the end plates.
The nutrient penetration stimulator is a dosed load that excludes static postures and great stresses. Physical inactivity is one of the main risk factors for thoracic osteochondrosis. Therefore, regular exercise is an important preventive measure.
The peculiarity of the microscopic structure - a few cells - reduces the intensity of regenerative ability and the rate of recovery of disc components. An anatomical feature is the weakness and lack of strength of the discs in the posterior sections. This contributes to the appearance of wedge-shaped discs in the lower thoracic and lumbar regions.
Great importance in the development of osteochondrosis is given to involutional changes. Actively degenerative changes begin to increase after 30 years. The synthesis of the components necessary for the disc (glycosaminoglycans) continues, but their quality deteriorates. Hydrophilia decreases, fibrosity increases, sclerosis appears.
Stages of intervertebral disc degeneration:
- prolonged asymptomatic course, degenerative changes in intradiscal components, displacement of the nucleus inside the disc;
- pronounced root symptoms of thoracic osteochondrosis, compression of the spinal cord, protrusion of the nucleus pulposus (protrusion, 1 degree);
- disc rupture with hernial protrusion (hernia, 2nd degree);
- degenerative changes in extradiscal components (grade 3).
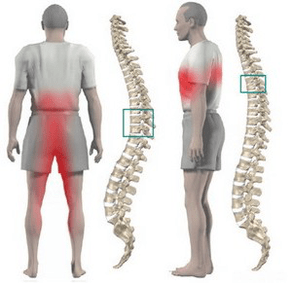
Pathological protrusion compresses nerve roots, blood vessels or spinal cord at different levels (cervical, thoracic, lumbar), which determines the clinical picture.
The restriction of the mobility of the thoracic spine, due to the presence of the thorax, contributes to the least traumatization of the intervertebral discs, and therefore to osteochondrosis. Physiological thoracic kyphosis contributes to the redistribution of weight from the upper half of the body to the lateral and anterior sections of the vertebrae. As a result, intervertebral hernias and osteophytes form on the anterior and lateral surfaces of the spine. Posterior osteophytes and hernias are extremely rare.
Osteochondrosis contributes to the narrowing of the intervertebral foramina and the compression of the roots of the spinal cord and sympathetic fibers. Sympathetic fibers arise from the gray matter of the spinal cord, then gather into nodes, from which they are sent to all internal organs. This leads to the fact that thoracic osteochondrosis, in addition to typical neurological disorders, leads to dysfunction of internal organs (vegetative, vasomotor, trophic) and imitation of somatic diseases. This feature of osteochondrosis of the thoracic discs explains the difficulties in diagnosing and prescribing the appropriate treatment.
Symptoms of chest osteochondrosis
Thoracic osteochondrosis is more typical of people with a sedentary lifestyle. At the same time, there is no stimulating effect of metered loads on the spine, which contributes to the disruption of disc recovery. Diseases develop in people who work at a computer for a long time, stoop, etc. such people should perform therapeutic exercises independently.
Most often, thoracic osteochondrosis is manifested by dull pains, less often aching and burning. The pain is localized between the shoulder blades. The patient is disturbed by the feeling of compression of the chest. When feeling the spinous processes of the thoracic vertebrae, local pain is detected, which increases with axial loads on the spine, deep inspiration and bends of the body.
A number of patients have sharp pains in the shoulder blade and lower chest (posterior costal syndrome). This symptomatology develops as a result of displacement of the lower ribs. The pain increases sharply when rotating the torso. Most often, the pain syndrome disappears abruptly.
Often the pain in the chest becomes a belt, corresponds to the course of the intercostal nerve. Sensitivity in the zone of innervation of the corresponding nerve ending is disturbed, paresthesias appear, and often there is a decrease in superficial and deep sensitivity. Possible violation of the function of the abdominal press, changes in knee and calcaneal tendon reflexes.
Violation of the function of internal organs occurs when a nerve root is compressed at the level of 1-12 chest. In the thoracic region there are structures responsible for the innervation of the lungs, heart, intestines, liver, pancreas and kidneys. Therefore, there are no signs characteristic only of thoracic osteochondrosis.
The disease is manifested by symptoms characteristic of another pathology:
- difficulty breathing;
- intense night pains;
- "heart", anginal pains;
- pain in the mammary glands;
- pain in the right or left hypochondrium (symptoms of cholecystitis and pancreatitis);
- pain in the throat and esophagus;
- pain in the epigastrium, abdomen (symptoms of gastritis, enteritis and colitis);
- sexual dysfunction.
Diagnostic
The greatest value in the diagnosis of thoracic osteochondrosis is an x-ray examination of the chest. The photo shows a decrease in the height of the intervertebral disc, terminal plaque sclerosis, the formation of osteophytes.
Computed tomography allows you to clarify the condition of the vertebrae, the joints of the spine, the size of the spinal canal, to determine the location of the hernial protrusion and its size.
When carrying out the differential diagnosis, it is necessary to carefully collect an anamnesis and compare all the clinical signs of thoracic osteochondrosis with the symptoms of other diseases. For example: heart pain with osteochondrosis is not stopped by nitroglycerin, epigastric pain is not associated with food intake, is not seasonal, all symptoms appear mainly in the evening and completely disappear after a night's rest.
How to treat thoracic osteochondrosis?
Treatment of osteochondrosis of the thoracic spine in almost all cases is conservative. The therapeutic indication is the predominance of visceral syndromes with neurological disorders. The primary orthopedic treatment should be adequate spinal traction:
- active vertical traction underwater;
- passive horizontal traction in inclined bed using the Glisson loop in case of lesion at the level of 1 to 4 thoracic vertebrae, by the axillary straps in case of lesion at the level of 4 to 12 thoracic vertebrae.
Drug treatment consists of performing paravertebral blocks with a solution of novocaine. With an exacerbation of the disease, painkillers and sedatives are used. With an unexpressed pain syndrome, it is permissible to use ointments with painkillers and anti-inflammatory drugs at home.
After the elimination of acute phenomena, a massage of the muscles of the back and lower extremities is used. Manual therapy is indicated for 1-3 degrees of osteochondrosis in the case of the development of functional blockages. It includes various options for soft and rough effects on the back muscles.
Therapeutic exercise allows you to load all parts of the spine in a dosed manner, which stimulates recovery processes. An important condition for exercise therapy of osteochondrosis is to exclude vertical loads.
Physiotherapy: UHF treatment, ultrasound, inductothermy, radon and pine-coniferous salt baths. At the spa stage, underwater traction and hydromassage are actively used.
Surgical treatment is rarely used. The indication for surgery is compression of the spinal cord by a prolapsed disc fragment.

















































